Humanising Digital Consent in Maternity Care
.png)
15 Min read
My role
Lead UX and Service Designer
As the primary designer on Re:Consent, I led the project from research to delivery across a full human-centred and trauma-informed design process.


Duration - 3 Months
-
Discovery + AI-supported research
• Interviews + field insights
• Systems mapping (journeys, blueprints)
• UX + content design
• Human–AI interaction flows
• Illustrations + visual system
• Prototyping (Figma, UX Pilot, Genially)
• Usability testing & iteration
What did I do?
Overview
Re:Consent reimagines how consent is communicated in maternity care. It introduces an interactive, trauma-informed consent walkthrough that prepares parents before labour, supports shared decisions during birth, and offers reflection tools after delivery. Restoring clarity, trust, and emotional safety in maternity care
Probelm Statment
Consent during childbirth is often rushed, unclear, and emotionally overwhelming. Families frequently feel excluded from urgent medical decisions, unsure of what is happening or why. At the same time, clinicians work under intense time and communication pressures, balancing clinical safety with empathy.These systemic gaps between intention and understanding contribute to birth-related trauma and a growing loss of trust between parents and care providers.
This project is transitioning into a standalone website. While it is in progress, the full PPT has been added to provide a complete overview of the work.

How we are bridging the gap ?
By Restoring agency, trust, and emotional closure before , during and after birth..
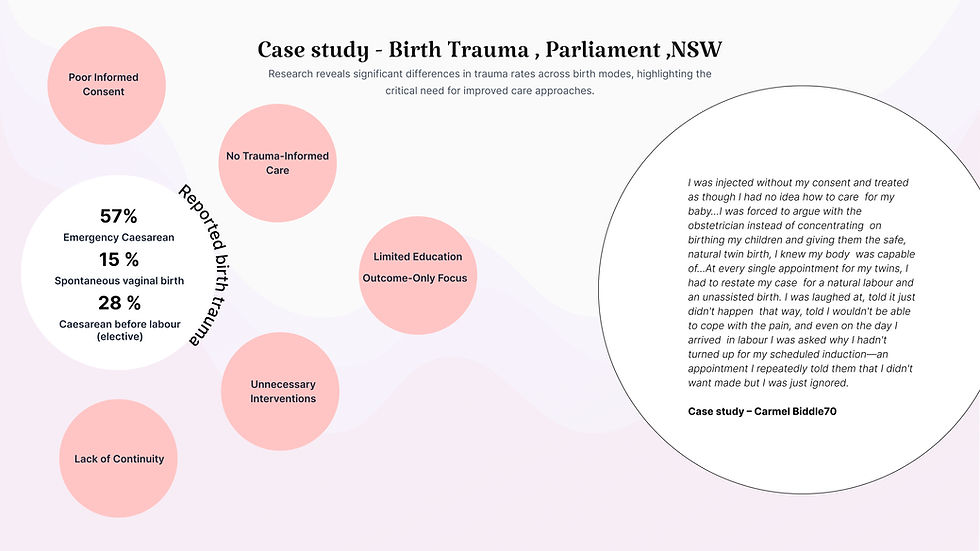
Why are we focusing Consent ? In material health care ?
Research shows most birth trauma stems from poor communication and lack of informed consent.

“We focus on consent because it is the leverage point that transforms communication, restores trust, and prevents trauma across maternity and beyond.”
Consent acts as the “moment of truth” where rights, trust, and care meet.
Health systems enforce safety protocols but neglect tools for shared decision-making and partner inclusion.
leverage point that improves communication, reduces trauma, and scales beyond maternity into surgery, emergency, and end-of-life care.

Discovery
I began with a landscape analysis of global clinical standards , including WHO Quality of Care , NHS personalised care guidelines, The National Safety , Quality Health Service (NSQHS) Standards and https://www.digitalhealth.gov.au/ . This revealed a fundamental misalignment. Current maternity consent practices rely on static artefacts such as PDFs, generic birth plans, and one-off verbal explanations. These tools do not adapt to clinical change, do not support shared decision making, and do not close the loop after birth. I also identified technological fragmentation across GP systems, hospital EMRs, and midwifery workflows.
So what is the Impact of Absent Shared Decision-Making,
Informed Decision-Making , Consent and lack of continuity in care in Maternity Care ?


Define
Through qualitative interviews with obstetricians, midwives, mothers, and partners, I surfaced deeper behavioural and emotional drivers. Themes included time scarcity, cognitive overload, lack of anticipatory guidance, and the absence of trauma informed communication. Importantly, I found that partners felt excluded and clinicians lacked tools that operationalise empathy within their time constraints. These insights informed a reframing of consent as an ongoing dialogue, not a one-time signature.
Research Highlights (From Field Interviews)
I had the opportunity to interview obstetricians, the clinical director, and senior midwives at the Royal Women’s Hospital, meeting with them multiple times over three months. Alongside this, I interviewed mothers, partners, and CALD participants, analysed trauma reports, reviewed podcasts, and gathered insights from five close friends and family members. I also drew on my own lived experiences to deepen the research.
Interviews with mothers and Partners

-
Rushed or unclear communication: Mothers felt they had “no time to ask questions” — 73% felt rushed during 10–15 minute consults.
-
Emotional safety: Unclear or contradictory explanations caused anxiety — 9 out of 15 reported feeling unsafe.
-
Need for visual clarity: Visuals improved understanding — 12 out of 15 preferred diagrams and scenarios over text.
-
Partner involvement: Partner exclusion increased stress — 11 out of 15 wanted partners to receive the same explanations.
-
Difficulty processing birth events: Emergency decisions blurred memory — 80% couldn’t recall parts of labour.
-
Language + literacy barriers (CALD): Medical terms were overwhelming — all 5 CALD participants struggled with terminology.
-
No emotional closer during postnatal
Interviews with Clinicians & Midwives
-
Time pressure: Consults are too short for deep consent conversations - typically just 10–12 minutes.
-
Emergency limits: Consent is often rushed - decisions made in 5–20 minute windows
-
Need for visuals: Scenario-based consent reduces fear — clinicians prefer visual explanation tools.
-
Emotional labour load: Midwives bear the weight of reassurance — 60–70% of time spent on support and admin.
-
Reassurance over data: Tone matters more than facts — “Reassurance is 50 percent of care.”
-
Missing reflection: Postnatal debriefs are rare — only 0–1 structured sessions unless requested.
-
Trauma-informed need: Trust hinges on empathetic delivery — all midwives flagged tone as critical.

The Gap: Fragmented and Systemic Break in Maternity Care
Current tools only cover isolated moments:
Antenatal → PDFs for education
Intrapartum → Consent forms during labour
Postnatal → EMR notes
This creates a fragmented experience. Families get information in disconnected bursts, with no emotional or informational clarity across the journey.
Even advanced platforms - EIDO, Concentric, TeamBirth, Babyscripts remain siloed. They address single slices, not the full journey.
This lack of continuity is the leverage point I focused on: closing the loop and turning fragmented touchpoints into a connected, reassuring care experience that supports both emotional well-being and informed decision-making throughout the entire journey.
How might we reimagine maternity consent as a continuous, trauma-informed journey , preparing mothers and partners in advance, supporting them in the moment, and ensuring clarity and trust after birth?
Define + Opportunity Space
“When I synthesised the thematic insights from mothers, partners, obstetricians, and midwives, I realised that the core problem was not lack of information but lack of emotionally safe, continuous, and shared communication. Consent was happening too late, too fast, and too narrowly reduced to signatures rather than understanding. Each insight exposed a structural gap: rushed appointments, fragmented explanations, partners excluded, and no postnatal reflection. These became the foundation of Re:Consent. From this analysis, the opportunity space became clear. I saw the need to shift consent upstream into antenatal care where decisions can be practised before stress sets in. I recognised that transparency must be built into the entire system, not just a single touchpoint. And I understood that any solution must work within 10-minute appointments while still supporting deep emotional needs. By reframing consent as a continuous journey rather than a one-off moment, I could design a service that strengthens shared decision making, rebuilds trust, and supports families across antenatal, intrapartum, and postnatal care. This opportunity space positioned Re:Consent as a bridge between empathy and efficiency, aligning with WHO respectful maternity care standards and the BRAIN framework for informed birth decisions. Re:Consent ultimately emerges from this insight: when communication becomes clear, structured, and trauma-informed, consent transforms from a rushed obligation into a shared safeguard that empowers mothers, partners, and clinicians alike.”
Develop
Through I prototyped an integrated service ecosystem that reframes consent as a continuous, connected, and emotionally safe experience. The solution comprises four core components: early-stage learning modules that scaffold understanding, a dynamic e-consent tool that supports real-time decision-making, a unified document hub that enhances continuity across touchpoints, and an AI-generated reflection kit that guides structured postnatal debriefing.
This continuous consent journey was developed using trauma‑informed language standards (WHO, NHS BRAIN) and iterated with 15 participants to validate emotional clarity, usability, and clinical realism. I also showcased the prototype at the Royal Women’s Hospital in Melbourne, gathering feedback from obstetricians and midwives to ensure the system aligned with real clinical workflows and frontline needs.
By treating consent not as a legal transaction but as a communication and behavioural design challenge, the system bridges clinical constraints with human experience, creating a safer and more supportive decision‑making environment.
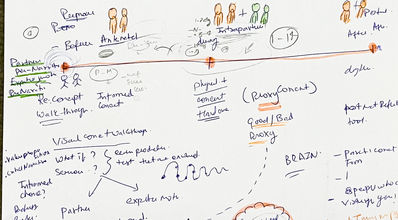
Expletory design development
Before beginning the Re:Consent project, my approach was intentionally broad and exploratory. Initially, I envisioned creating a physical intervention something tactile that could exist within hospitals to support communication and consent. This early phase focused on “brain-to-hand” design through sketches and paper-based prototyping to visualise the maternal care journey. However, as the exploration progressed, several practical limitations emerged. Physical artefacts within hospital environments presented significant hygiene and management challenges, and maintaining cleanliness across shared objects became unrealistic in postnatal and labour settings. Through conversations with peers and clinical references, I also identified a recurring pain point: mothers and families are already overwhelmed by numerous physical materials such as brochures, consent papers, and printed guides. These are often fragmented, easily lost, and rarely revisited. As the healthcare system moves toward digitisation of records and education, it became evident that a digital solution would provide more flexibility, continuity, and accessibility. I therefore transitioned the concept into a digital design space, allowing for iterative refinement and real-time adaptability. Early journey maps and consent flows were still hand-drawn on paper to establish logic and narrative clarity. Once the structure was validated, I developed a digital prototype, which proved easier to iterate, manage, and integrate with existing hospital systems. This shift from physical to digital not only improved practicality but also aligned with contemporary trends in connected, trauma-informed healthcare design.

As the project grew in complexity, I structured Re:Consent as a single service system rather than isolated features. I mapped key breakdown points across pregnancy where anxiety is high, time is limited, and consent often becomes unclear. This led to a three-phase framework aligned with how people actually experience care: before, during, and after birth.
The framework adapts interactions to users’ cognitive and emotional capacity at each stage. Visual walkthroughs support preparation before birth, critical prompts reduce decision fog during birth, and the Reflection Kit provides closure after birth.
This structure guided all UI decisions and system flows, ensuring clarity, empathy, and shared decision-making throughout the journey.
AI-Assisted Content Strategy and UX Workflow
To accelerate a complex project with many clinical pathways, I used AI as a UX pilot while keeping full control of the design direction. I first defined the system framework and information architecture for Re:Consent, then used a master prompt (“vibe code”) to generate early content for scenarios and screens. AI often produced excess or misaligned information, so I curated and refined it carefully. Around 60 percent of the generated content was usable after restructuring it into my trauma-informed IA. This workflow helped me manage time under a tight deadline while still designing clear, human-centred interfaces across high-pressure procedures such as NIPT, amniocentesis, emergency C-section and stillbirth care.
Designing a Trauma-Informed Prototype to Reduce Decision Fog
To accelerate a complex project with many clinical pathways, I used AI as a UX pilot while keeping full control of the design direction. I first defined the system framework and information architecture for Re:Consent, then used a master prompt (“vibe code”) to generate early content for scenarios and screens. AI often produced excess or misaligned information, so I curated and refined it carefully. Around 60 percent of the generated content was usable after restructuring it into my trauma-informed IA. This workflow helped me manage time under a tight deadline while still designing clear, human-centred interfaces across high-pressure procedures such as NIPT, amniocentesis, emergency C-section and stillbirth care.












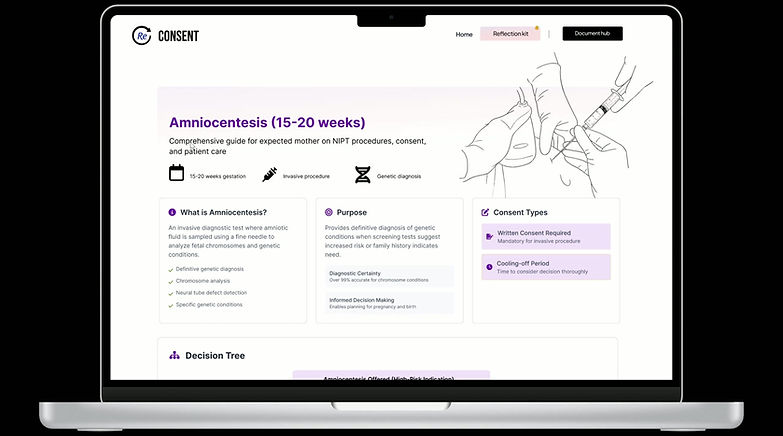
Learning Modules - Scenario-Based Education
Interactive flip cards and “What-if” walkthroughs prepare parents for real decisions before labour begins. They replace overwhelming PDFs with calm, visual learning - empowering both parents to engage early and equally.
I designed the learning modules to cover the full maternity journey, but I intentionally focused on the moments where communication breaks down most. After mapping all antenatal, intrapartum, and postnatal procedures, I narrowed the scope to the high-stakes points clinicians and mothers identified as the most confusing: NIPT, amniocentesis, instrumental delivery, emergency caesarean, stillbirth, feeding choices, and contraception after birth.
To keep information consistent, I applied the NHS BRAIN framework — Benefits, Risks, Alternatives, Intuition, and Next or Nothing and developed an information architecture framework for this project according to pain points and needs... This gave every module a clear rhythm and helped me translate clinical complexity into calm, trauma-informed, and emotionally safe content for both mothers and partners.
User Interface Reflection
I designed the interface to lower cognitive load and reduce anxiety. The visual hierarchy is soft and simple, and the line drawing illustrations help keep the experience grounded without feeling clinical. I used long-scroll pages instead of multi-step clicking because it lets users follow the story at their own pace. The decision tree, Q&A blocks, and conversation prompts give both mother and partner a structured way to understand options and prepare for discussions with clinicians.
Information Architecture (IA)
I structured each procedure page to feel predictable and supportive: • Header: simple navigation for Home, Procedures, Mother View, Partner View • Overview: a short, empathetic explanation of the procedure • Summary Cards: what it is, why it happens, consent types • Decision Tree: shows how choices unfold in real time • Care Information: before, during, and after the procedure • BRAIN Framework: clear benefits, risks, and alternatives • Emotional Experience: mother and partner perspectives • Recovery: practical timelines and safety guidance • Conversation Prompts: questions to ask clinicians • Illustrations: minimal, calm visuals to reduce stress This structure allowed me to hold emotional complexity while keeping the experience extremely clear.
Using AI for Content Development
To build consistent, trauma-informed content, I used GPT and RMIT’s VAL platform as part of a structured writing workflow. I designed prompts that aligned with clinical guidelines and decision-making frameworks, then refined AI-generated text through human judgment and research. Across all modules, I created twelve decision trees and used AI to help organise tone, flow, and clarity — but I kept all final decisions grounded in ethics, accuracy, and lived experience insights.
Why This Approach Works
By narrowing the scope to the most emotionally fragile moments, and pairing it with trauma-informed language, clear IA, and structured decision-making support, I transformed overwhelming clinical procedures into calm, human, and accessible guidance. This approach keeps the system usable for families, feasible for clinicians, and scalable across any future medical procedure.

Dynamic E-Consent Tool - Real-Time Decisions During Labour
Interactive flip cards and “What-if” walkthroughs prepare parents for real decisions before labour begins. They replace overwhelming PDFs with calm, visual learning - empowering both parents to engage early and equally.
I designed the learning modules to cover the full maternity journey, but I intentionally focused on the moments where communication breaks down most. After mapping all antenatal, intrapartum, and postnatal procedures, I narrowed the scope to the high-stakes points clinicians and mothers identified as the most confusing: NIPT, amniocentesis, instrumental delivery, emergency caesarean, stillbirth, feeding choices, and contraception after birth.
To keep information consistent, I applied the NHS BRAIN framework — Benefits, Risks, Alternatives, Intuition, and Next or Nothing and developed an information architecture framework for this project according to pain points and needs... This gave every module a clear rhythm and helped me translate clinical complexity into calm, trauma-informed, and emotionally safe content for both mothers and partners.
User Interface Reflection
I designed the interface to lower cognitive load and reduce anxiety. The visual hierarchy is soft and simple, and the line drawing illustrations help keep the experience grounded without feeling clinical. I used long-scroll pages instead of multi-step clicking because it lets users follow the story at their own pace. The decision tree, Q&A blocks, and conversation prompts give both mother and partner a structured way to understand options and prepare for discussions with clinicians.
Information Architecture (IA)
I structured each procedure page to feel predictable and supportive: • Header: simple navigation for Home, Procedures, Mother View, Partner View • Overview: a short, empathetic explanation of the procedure • Summary Cards: what it is, why it happens, consent types • Decision Tree: shows how choices unfold in real time • Care Information: before, during, and after the procedure • BRAIN Framework: clear benefits, risks, and alternatives • Emotional Experience: mother and partner perspectives • Recovery: practical timelines and safety guidance • Conversation Prompts: questions to ask clinicians • Illustrations: minimal, calm visuals to reduce stress This structure allowed me to hold emotional complexity while keeping the experience extremely clear.
Using AI for Content Development
To build consistent, trauma-informed content, I used GPT and RMIT’s VAL platform as part of a structured writing workflow. I designed prompts that aligned with clinical guidelines and decision-making frameworks, then refined AI-generated text through human judgment and research. Across all modules, I created twelve decision trees and used AI to help organise tone, flow, and clarity — but I kept all final decisions grounded in ethics, accuracy, and lived experience insights.
Why This Approach Works
By narrowing the scope to the most emotionally fragile moments, and pairing it with trauma-informed language, clear IA, and structured decision-making support, I transformed overwhelming clinical procedures into calm, human, and accessible guidance. This approach keeps the system usable for families, feasible for clinicians, and scalable across any future medical procedure.